Being the best at getting better – our learning & improvement community
Blog written by

Samantha Allen, chief executive, North East and North Cumbria Integrated Care Board

Annie Laverty, executive director improvement and experience, North East and North Cumbria Integrated Care Board
About the North East and North Cumbria Integrated Care System
North East and North Cumbria is one of 42 integrated care systems (ICSs) and the largest in England responsible for more than three million people across 5,313 square miles. Across our region people face significant health challenges; from some of the highest rates of heart disease, liver disease and suicide in England, disparities in life expectancy and rates of child poverty that are double the England average in some areas.
ICSs first started back in 2016 and to begin with were quite informal. This changed in 2022 with the new Health and Care Act which created an Integrated Care Board (ICB) and an Integrated Care Partnership (ICP) both of which are focused on creating the ambition and infrastructure, working with partners including local government, the voluntary, community and social enterprise sector, NHS and others, to achieve integrated care across the area served.
Established in July 2022 ICBs have four purposes, improve outcomes in population health and healthcare, tackling inequalities in outcomes, experience and access, enhancing productivity and value for money and helping the NHS support social and economic development (NHS England) .
The ICP, established in 2022, is a joint committee which brings together all system partners to develop a health and care strategy for the area. Our ICP has recently signed off an integrated care strategy for our region called Better Health and Wellbeing for All. This strategy sets out four ambitious goals to reduce inequalities in life expectancy, ensure fairer outcomes for all, deliver better health and care services and giving our children and young people the best start in life.
Building our learning and improvement community
Evidence tells us that connectedness and strong, trusting relationships matter for improvement. Analysis of high performing systems shows how strongly connected networks create a capacity to facilitate knowledge exchange for innovation and improvement across a system. So even before the ICS was established, we set out to build a learning and improvement community. For us, setting up the ICS to act as a system convenor, helping to connect people and build relationships across the system, with people united by shared goals for improvement, wasn’t just a priority, it was a precondition for success.
A learning community can be described as: ‘A group of peers who come together in a safe space to reflect and share their judgements and uncertainties about their practice and to share ideas or experiences to collectively improve.’ (Lowe and Wilson). There was already a long history of commitment to learning and improvement in the North East and North Cumbria. Some of the most pioneering and impactful improvement work in the NHS over the last two decades originated in our system. There are already many examples of transformational innovations and improvements in our system, across health, local government, community and voluntary sectors. Establishing the learning and improvement community created the opportunity for sharing, collaboration and amplification, so that the sum of the collective could be greater than the parts and make a difference to more of our population.
Inspired by Cincinnati Childrens, we adopted the ambition to “be the best at getting better”. As an integrated care system, we should be ambitious; we, naturally, want to be ‘the very best’ for those who use our services, for the whole population and for the people who work in our system. Our aspiration to ‘be the best getting better’ is, however, something that can unite us all. So rather than saying we want to “be the best” which feels like a faraway goal, we aspire to “be the best at getting better”. We seek to put improvement at the heart of everything we do as an ICS. We are utilising an improvement mindset and improvement methods to tackling our biggest challenges in health and healthcare. When we choose to continually prioritise ‘getting better’ we don’t give up when we make mistakes, or when a new situation arises that challenges our current knowledge, resources, and skill levels. Instead, we accept that we won’t always get it right, nor will we know everything. This leads us to adopt strategies that help us to acquire the skills and resources required to resolve the situation and achieve success.
Our ambition to “be the best at getting better” also means understanding what “best” means globally, as well as nationally, and aspiring to worldwide good practice. We seek to bring in international partners to all the key events of the learning and improvement community, learn from others and also share our learning generously. This is very much of the spirit the people who live and work across the North East and North Cumbria.
In order to create improvement across the system, we need to help build agency, the power that people need to be able to feel if they are going to make change. As well as engaging leaders with formal authority from every organisation in the ICS, we are seeking to develop a social movement that mobilises people with lived experience and people who work at the point of care. We aim to:
- co-produce all our activities and always give voice to and seek testimony from those who have less power in the formal system.
- make learning and improvement the default approach in how we go about tackling our biggest challenges as an ICS
- build a collective capability in learning and improvement that enables us to keep learning and growing as individuals, teams, communities, places and as a system and to get better at delivering our goals
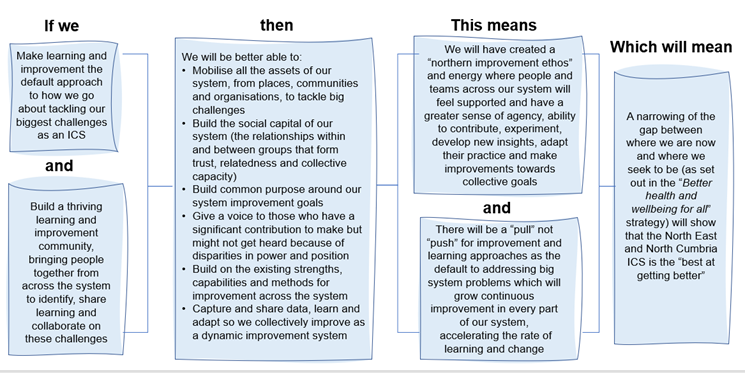
We are continuing to build a logic model for our learning and improvement strategy with partners from across our system. A logic model is an explicit statement of the activities that we believe will bring about change and the results we hope to see for the community and its people
A logic model for the North East and North Cumbria learning and improvement community
We are working with the Health Foundation (where we have secured over £200k funding to support this work) and an evaluation team from the University of Newcastle to define and test measures of strategic impact for our learning and improvement community. These may include:
- Strategy goal improvement at accelerated rate
- Use of learning and improvement approaches
- Levels of engagement
- Number of improvement ideas to implementation
- Sense of shared purpose and belonging
- Growth of social capital
We have created a governance system that includes bi-monthly meetings of an active steering group, with representatives from across the system, including people with lived experience and their advocates as well as leaders from the formal system.
How we are implementing our approach
We held the inaugural meeting of the North East and North Cumbria learning and improvement community on 21 September 2022. Over 200 people from across the region participated with the objective of co-creating a learning and improvement system.
Through a structured co-creation process, seven priority areas were identified for the improvement and learning community to work on together:
- Mental health services for children and young people: access and crisis support
- Collaborative leadership – what does it look like? How do we do it efficiently?
- Shifting the balance from treatment to prevention
- How do we share learning and join up what we are doing as a system?
- How can we build and develop our social care workforce?
- The retention and wellbeing of people who work in our system
- Safe transfers of care, particularly from hospitals
We are moving forward with each of these priorities in a way that reflects the spirit of the learning and improvement community. An example is the work on safe transfers of care. On 9 March 2023, the learning and improvement community hosted a “discharge summit”. Three hundred people signed up. The summit was co-created by a design team that represented many different interests and perspectives. The design team wanted the summit to build on and amplify the strengths of existing successful practice within North East and North Cumbria ICS. 70% of the content that was showcased at the summit came from within the system. In addition, there were inputs from national experts, such as an opportunity to work with the national NHS Behavioural Insights team exploring “Which behavioural biases might influence the decisions clinicians make about hospital discharge, and how should we address these biases?” as well as contributions from global leaders from the US and Sweden, discussing their approaches to transfers of care.
The feedback from participants was overwhelmingly positive, with many new connections being made and commitments to taking action. The summit felt very different to previous collaborations to improve the flow of people through the system. It did not just involve people from the formal system who are responsible for service delivery. It also included people with the motivation and passion to take action, people with the voice of lived experience, people with the improvement skills who can help make a difference, people who can broker, facilitate and communicate, and people who can make connections with diverse communities. We need all these voices if we are to collectively deliver improvement across the system.
As a result of the discharge summit, a collaborative learning community has been established, with an initial focus on sharing good practice, co-production, and standardisation.
System improvements in urgent and emergency care
System leaders as part of our Urgent and Emergency Care (UEC) Strategic Board were able to agree and commit to three priorities for winter operating resilience in 2022/ 2023: 1) enhanced clinical triage 2) use of urgent primary care and 3) system flow. With a focus on learning together we have held three Community of Practice Events on (a) Enhanced clinical advice (b) Handovers and (c) Urgent Treatment Centres as well as two Winter planning events – all with clear actions, a commitment to deliver and attendance from up to 150 people per time.
Five interventions were piloted to support system UEC priorities. Whilst we have more to learn to inform winter planning in 2023/ 24 and to improve variation of delivery across all acute hospital trusts, the early evaluation of our system improvement work is very promising.
|
Intervention |
Impact |
|
111 online and call answering capacity |
44% reduction in call answering time |
|
Emergency department streaming |
2% reduction in emergency department attends (about 400 people per week) – further work required across the system to see in all locations but a promising start |
|
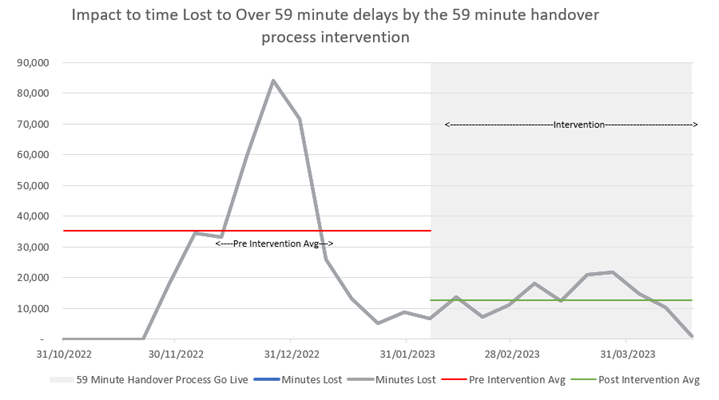
59 minute ambulance handover delay backstop |
Substantial 64% reduction in minutes lost to handover delays over 59 minutes since the intervention was implemented at an aggregate system level. |
|
Bed number increases with demand and capacity funding |
Weekly available bed days increased by 4% from an average of 40,988 to 42,756 - an extra available 1,768 bed days weekly. |
|
Community falls service |
6% decrease in falls-related admissions to hospital due to the community-based response services. From a care home perspective 12% decrease in admissions |
Building on a platform of collaborative relationships
At the heart of our North East and North Cumbria learning and improvement approach is a focus on collaborative relationships. Convening the community in this way enables us to help build a lot of new relationships and connections that did not exist before. Our aspiration is that this social connectedness, development of shared purpose and collaboration around change will make a positive difference for many people in our system and will be a conduit for delivering our Better Health and Wellbeing for All strategy. Value will be created and breakthroughs (in thinking, practice and outcomes) made through the strength, number and quality of relationships in our system. Through the work undertaken so far we have learnt there is far more that unites us across a large health and care system than divides us and people are highly motivated to make a difference for the communities they serve.
It is still early days for the learning and improvement community, but our experience so far suggests that these relationships may be key to unlocking the value we are seeking as a system.
May 2023
Find our more about our learning and improvement community







