
Becca Scott
Head of Public Health and prevention: NENC maternity services

Ros Nunn
Public Health practitioner and specialist infant feeding lead
Giving every child the best start in life (BSIL) is known to reduce health inequalities and in the aftermath of Covid-19 this is an essential key component of pandemic recovery. Too many children in the North of England do not have the best start in life that they need to thrive, and maternity care gives the first key opportunity to initiate positive change (Marmot, 2010).
The NENC LMNS Public Health and Prevention team leads on the strategic priorities of the NENC Integrated Care Board (ICB), the Maternity & Neonatal Single Delivery Plan (2023), the LMNS Equity & Equality Plan (2022), as well as supporting delivery of subsections of the NHS Long Term Plan (LTP) (2019) pertaining to the best start in life/maternity. The programme is being delivered through a core team working with the North East & North Cumbria system partners, Service Users, Clinicians, Directors of Public Health, Directors/Heads of Midwifery, Office of Health Inequalities & Disparities, Commissioners and researchers/academics.

Head of Public Health and prevention: NENC maternity services

Public Health practitioner and specialist infant feeding lead
Our purpose
Working with partners, pregnant persons and their support systems, improve equitable access, experience and outcomes in pregnancy and postnatal healthcare.
Objectives
Support services
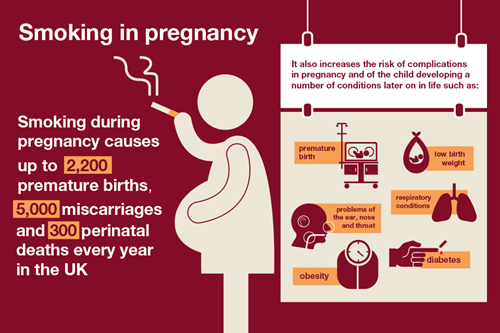
Around 3330 babies are born to mothers who are tobacco dependent each year in the North East & North Cumbria. Tobacco dependency is main modifiable risk factor for a range of poor pregnancy outcome it is strongly correlated to high neonatal admissions, still births, sudden infant deaths and low birth weight in the region.
Smoking in pregnancy imposes a considerable economic burden on society. Health care costs are imposed on the NHS, during pregnancy and in the year following birth, as a result of mothers continuing to smoke during pregnancy.
Costs to the NENC NHS related to maternal increased risk of miscarriage, ectopic pregnancy, placenta previa, abruption of the placenta, preterm premature rupture of membranes and decreased risk of pre-eclampsia are estimated to be £10.2 million per year. In addition, costs related to infants’ increased risk of preterm delivery, low birth weight, Sudden Infant Death Syndrome, perinatal mortality, asthma, otitis media, and upper and lower respiratory infections are estimated to be between £12 million and £23.5 million per year based on different costing methodologies.
It is possible to generate positive economic cost savings by introducing low-cost smoking cessation interventions during pregnancy. It is estimated that spending between £13.60 and £37 per pregnant smoker would yield positive cost savings for the NHS. This is purely in economic terms and does not include the health benefits to mothers and children. These cost estimates are conservative and are limited to NHS costs during pregnancy and the first year of life.
Some women continue smoking during pregnancy despite the extensive information available on the dangers smoking poses to their unborn child. Moral judgements are commonly directed to mothers through reference health behavior in pregnancy. The reasons for mothers continuing to smoke during pregnancy are complex but the reality is that smoking in pregnancy is not a lifestyle choice. The Royal College of Physicians’ report on nicotine addiction states that “it is reasonable to conclude that nicotine delivered through tobacco smoke should be regarded as an addictive drug, and tobacco use as the means of self-administration”. They conclude that: “Cigarettes are highly efficient nicotine delivery devices and are as addictive as drugs such as heroin or cocaine.” It would therefore be more pertinent to refer to all smoking as tobacco dependency, a condition in which requires medicalised support.
All North East and North Cumbria Maternity services have trained support workers who can advise further, read more information here.
In addition to this, there is free access to all features in the Smoke Free App (RRP £90), view here.
Support information
Stop smoking in pregnancy here
View the infographics and materials here.

All Maternity, Neonatal Units and 0-19 services in the North East and North Cumbria have Infant feeding Leads, or Champions who can give 1:1 support and advice to both colleagues and families.
All localities have varying services through support groups and in some areas peer support, information can be accessed from 0-19 services.
Information on breastfeeding, bottle feeding, feeding a preterm baby, feeding twins and multiples, Expression and storage of breastmilk:
Association of breastfeeding mothers
Drugs in Breastmilk information
Breastfeeding Network - drugs in breastmilk
Special Pharmacy Services - Breastfeeding medicines advice service
Formula Milk and information on mother and infant nutrition:
First steps nutrition
First steps nutrition - infant milks
First steps nutrition - parents and carers
These helplines are all run by trained volunteers for breastfeeding people:
National Breastfeeding Helpline - 0300 100 0212 (available every day, 9:30am to 9:30pm).
In Bengali/Sylheti 0300 456 2421; in Tamil, Telugu and Hindi 0300 330 5469
NCT Breastfeeding Line - 0300 330 0771 (available 8am to midnight)
La Leche League 0345 120 2918 (This is open from 8am to 11pm, 365 days a year)
Better Health, Start for Life infant feeding hub resources here.
UNICEF Baby Friendly Initiative here.
For information in several different languages visit here.
Best Beginnings – films and app for parents to be and new parents here.
Pregnancy, childbirth and the new-born period can be a stressful time and can trigger pre-existing or new mental health problems. The following resources from the NHS, professional bodies and national charities can be very helpful to provide information and support surrounding mental wellbeing, view them here.
Support for parents
Mind - Parenting and mental health
NCT - Emotions during pregnancy
Tommy's - Emotional changes in pregnancy
NHS - Mental health and pregnancy
Support for dads
Dads Matter UK - Getting support for yourself
The Book of Man - Postnatal depression in men
Support for young dads
Managed by the North East Young Dads and Lads Project (NEYDL), DigiDad is an online E-learning platform made by young dads for young dads and featuring father-friendly films, podcasts and training materials to support young men on their journey to fatherhood and beyond, see here.
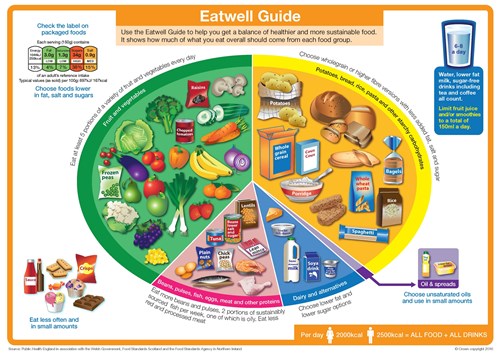
Best Start in Life recognises that from preconception through to 6-8 weeks following the birth of a baby the healthier a mother is, the better outcomes for both them and the infant. Mothers who have overweight or obesity have significantly increased risks including difficulty conceiving, miscarriage, gestational diabetes, thromboembolism, pre-eclampsia, instrumental / Caesarean delivery. Whilst risk for babies include preterm birth, stillbirth, small or large-for gestational-age, congenital anomalies, perinatal death / sudden unexplained death in infancy and childhood obesity. Eating healthily and keeping active can help in maintaining and achieving a healthy weight.
Eat Well Guide (PHE 2016) see here.
Healthy eating in pregnancy (Better Health 2022) see here.
British Dietetic Association food portion guides can support balancing meal/plate quantity, see here.
Eating well in pregnancy see here.
Eating well for new Mums (including information for breastfeeding mothers) see here.
NHS Start4Life - Health eating pregnancy
Physical Activity
NHS Start4Life - Exercising in pregnancy
Advice on activity and sport can be found here.
Infographics


Ensuring that families achieve and maintain good health throughout their reproductive years and beyond will not only impact their health, it will also influence the health of future generations
A planned pregnancy with effective preconception care improves health and reduces the risk of infants being born prematurely, having a low birth weight, reduces the incidence of birth defects and birth-related conditions that could negatively impact on a child’s optimal development.
By providing tailored care, education and appropriate support prior to, during and post pregnancies to individuals and their families who have conditions and behaviours that have been identified as having a negative impact on their health, their family’s health and their home environment we can positively influence lifelong health and wellbeing.
The Chief Medical Officers for the UK recommend that during pregnancy or when planning to become pregnant, the safest approach is not to drink alcohol at all to keep risks to unborn babies to a minimum. Drinking alcohol in pregnancy can lead to long-term harm to the baby.
Fetal Alcohol Spectrum Disorder (FASD) refers to the range of neurodevelopmental problems caused by pre-natal exposure to alcohol. The effects are diverse and impact on the individual throughout their life course.
Royal College of Obstetricians and Gynaecologists - Alcohol and pregnancy
Screening information for pregnant people and babies here.
Pregnancy and Birth Choices in the North East and North Cumbria App here.
Data and intelligence
This digital resource aims to bring together maternity information from a range of sources and supports the maternity transformation programme, see here.
This brings together a range of publicly available data, information, reports, tools and resources on child and maternal health into one easily accessible hub. It helps you find and use the information and evidence you need to improve decision making as part of your planning or commissioning process, see here.
This tool is designed to bring together available data on obesity and the conditions associated with it, to assist in developing an integrated approach to addressing obesity in local areas, see here.
Poverty Proofing© devised by Children North East (CNE) is a powerful tool designed to help remove the barriers and alleviate the impact those in poverty face when accessing key organisations and services. This work was carried out with James Cook University Hospital, Middlesbrough. It started in July 2023 and ended in April 2024. The focus was on the ‘booking assessment,’ which is the first appointment a woman or person has with a midwife when they find out they are pregnant. There is confusion around booking this initial appointment. People need to register their pregnancy using a digital app (BadgerNet), but the act of registering does not automatically create an appointment with the midwife, as many people believed. It is examples like this that then cause delays from first registering to actually seeing the midwife, which is something this project aims to remove/reduce. Whilst every effort was made to focus on this, Poverty Proofing© is led by people and naturally other elements of the maternity journey came up in conversation. Where these topics were pertinent to poverty or had an element of financial exclusion, they were considered to be relevant to the service and were included in the report. CNE were commissioned to do this work through the North East and North Cumbria (NENC) Integrated Care Board’s (ICB) Healthy and Fairer Programme. This was established in September 2023 to achieve the NENC ICB goals of 'Longer and Healthier Lives', and 'Fairer Outcomes for All'. South Tees Maternity Service put itself forward to be an ‘exemplar pathway’ as part of this programme of work. Special thanks to all the staff, new and expectant parents both in clinic and in the community who helped to build up this rich picture of the maternity booking assessment in South Tees. This pathway is part of a wider piece of work involving digital inclusion and health literacy.
STAGE 1: Training and consultation with staff 41 staff in different job roles completed a three-hour training session.
STAGE 2: Scoping Time was spent gathering information about the setting and how it works. This stage included conversations with front line staff and management, observing interactions and reviewing key areas such as the website and communications.
STAGE 3: Patient and community consultations We spoke to 168 people in total. This included 101 people visiting the antenatal clinic at James Cook and 67 people in various community settings across the region. This included pregnant people and their families, and new parents.
STAGE 4: Feedback session. An initial feedback session was held with representatives from the NENC ICB, LMNS, Children North East, Health Literacy and Creative Health. This was followed up with a Booking Project Planning Session to consider solutions and recommendations going forward. We then produced this final report.
STAGE 5: A South Tees action plan has been developed and will be shared with local system partners to collaborate on improvements. The NENC ICB are developing a plan to share learning and make NENC improvements which will be overseen as part of the emerging LMNS Pregnancy Anticipatiry Care Delivery Group.
STAGE 6: Review 9 months after completion, CNE will return and complete a review, identifying impact, good practice and potential considerations moving forward.
Training
Train the trainer courses for health care professional are available through Northern LMS site training hub with restricted access. https://www.northernlms.org
E-learning for healthcare - Infant feeding
E-learning for healthcare - Breastmilk provision for preterm and sick neonates
E-learning for healthcare - New healthier weight
Active Pregnancy Foundation - This mum moves
If you a member of the Royal College of Midwives you can access the Professional and practice Module - Nutrition and Obesity – Obesity: Supporting women here.
Materials and resources
Birth reflection services in the North East of England report here.
North East and North Cumbria tobacco dependency in pregnancy pathway and script here.
North East and North Cumbria breastfeeding strategy here.
North East and North Cumbria infant feeding touchpoint pathway here.
Returning to work
NHS Start4Life - Going back to work
Health and Safety Executive - Pregnant workers and new mothers: Your health and safety
Returning to work letter for employers
Returning to work letter here.
The NENC Perinatal Mental Health Network’s Vision is that all women and birthing people, parents, partners and their babies in North East and North Cumbria experience optimum mental health and emotional wellbeing in the perinatal period through the provision of safe, equitable, integrated quality services. For mental health to be core business for all. For staff to be provided with the environment, resources and support to thrive in the workplace. For services to be coproduced with our service users and their families.
The NENC whole systems approach and pathway supports Maternity services to deliver this ambition.
North East and North Cumbria ICS perinatal mental health whole systems approach here.
PMH ICS self-assessment here.
PMH care passport here.
North East and North Cumbria ICS alcohol in pregnancy pathway here.
North East and North Cumbria alcohol screening in pregnancy tool here.
North East and North Cumbria alcohol screening in pregnancy professional guidance here.
The NENC ICS Planning a Pregnancy Resource Tool is an interactive resource tool that all professionals can use to signpost individuals to and for anyone who is thinking of starting a family/planning a pregnancy or who have recently had a baby. It has relevant, reliable pre-conceptual health advice in one place, making access to information easier for individuals planning to have a baby in the near or distant future.
Find the planning a pregnancy poster here.
Other useful information
NHS England single delivery plan
Local maternity and neonatal system equity and equality action plan
NHS Long Term Plan - maternity and neonatal services (2019)
NHSE&I Maternity Transformation programme
Marmot Review 10 years on (2020)
1001 Critical Days refresh (2021)
2024/25 NHS Priorities & Operational Planning Guidance
Clinical Negligence Scheme for Trusts
Saving Babies Lives Care Bundle (2019)
Maternity high impact area: Supporting parents to have a smoke free pregnancy. Read more here.
Maternity high impact area: Supporting healthy weight before and between pregnancies. Read more here.
Maternity high impact area: Supporting good parental mental health. Read more here.
Maternity high impact area: Improving planning and preparation for pregnancy. Read more here.
Maternity high impact area: Reducing the incidence of harms caused by alcohol in pregnancy. Read more here.
Maternity Voices Partnerships (MVP) are a team of women and their families, commissioners and providers, working together to review and contribute to the development of local maternity care. MVPs serve the needs of local women and families, gathering feedback and advising the Local Maternity Systems, Clinical Networks and those commissioning services from a service user perspective.
The Local Maternity Systems facilitate the co-production of services and transformation through the sustainable establishment and funding of Maternity Voices Partnerships and we host a Northern England wide forum, the Maternity Engagement group, bringing all MVPs together to influence and share in local decision-making.
For more information visit here.
To speak to our team or to be added to the stakeholder newsletter please email nencicb-cu.lmns@nhs.net
For media enquiries please contact necsu.comms@nhs.net